| Surgical technique: Posterior cervical foraminotomy | |
| Step | Key Points |
| Positioning | – Patient is positioned prone on a reversed OR table with a Mayfield head holder and chest bolsters. – Table inclined 20°–30° reverse Trendelenburg; Mayfield adjusted for neck flexion to reduce redundant skin and facilitate facet exposure. – Shoulders taped for radiographic localization. |
| Neuromonitoring | – Neuromonitoring generally unnecessary. |
| Incision localization | – Use external occipital protuberance, C2, and C7 spinous processes for incision landmarks. – Use a lateral C-arm x-ray prepped with a metallic marker on the skin. – Confirm levels intraoperatively with a lateral C-arm and spinal needle on the facet. |
| Approach | – Midline incision for bilateral; unilateral can use 2 cm lateral or midline incision. – Subperiosteal dissection to expose facet joint and lateral mass-laminar junction. – Expose more than 50% of the facet while considering the lateral edge location. |
| Retractor placement | – McCulloch retractor or alike with blade laterally and hook on the interspinous ligament. |
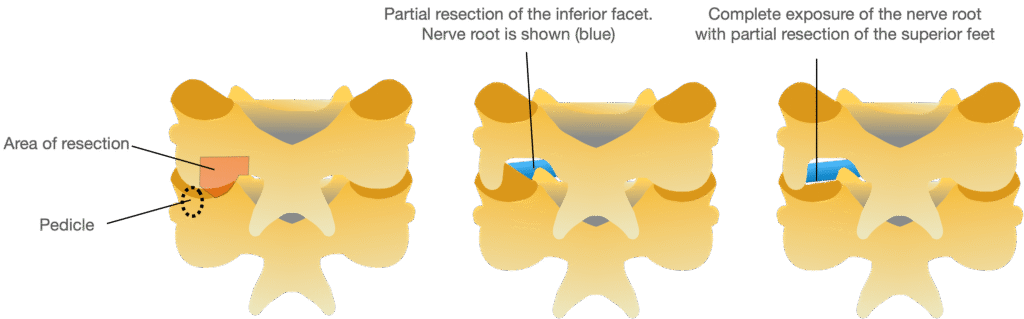
| Decompression technique | – Address compressive elements: superior articular process (SAP) and uncovertebral osteophyte/disk herniation. – Medial facet resection (50%) to uncover nerve root. – Burr thinning of inferior articular process of vertebra above until translucent; bone removed with curette or Kerrison rongeur. – Venous bleeding managed with gelfoam packing. |
| Discectomy | – Remove extruded fragments; manipulate nerve root if needed for intraforaminal herniations. – Cranial pedicle resection possible for access with microsurgical instruments. |
| Closure | – No drain required. – Deep muscle and fascial layers closed with Vicryl figure-of-eight sutures; dermal and skin layers closed with Vicryl and subcuticular Monocryl sutures. |
| Postoperative care | – Detailed neurological exam post-op. – Optional soft collar for less than 2 weeks. – Resume range of motion as tolerated. |